Introduction to Pelvic Floor Therapy
If you would have told me when I was in physical therapy school that I would one day be a pelvic floor physical therapist, I would have thought you were crazy. It wasn’t until I became pregnant with my daughter and found postpartum recovery to be difficult that I decided to seek pelvic floor therapy for myself. I am forever grateful to that physical therapist for helping me with my concerns and guiding me towards an area of treatment that I previously never would have considered.
What exactly is the pelvic floor?
The pelvic floor is made up of 3 layers of muscles as well as other connective tissues. The muscles span from your pubic bone at the front of your pelvis to your tailbone at the back of your pelvis, as well as in between your SITS bones (the bones that get sore when you sit on the bleachers at a sporting event).
Why do we have different layers of pelvic floor muscle?
Each layer of pelvic floor muscle has a specific function:
Superficial Layer of Pelvic Floor image from https://thevagwhisperer.com/2020/05/08/what-is-a-pelvic-floor-anywaynbsp/
The first layer is the superficial layer, which is the outermost layer of muscle and is just underneath your skin. These muscles contribute to arousal, orgasm, and the ability to voluntarily hold back urine.
The second layer is the middle layer. These muscles support your urethra and help with bladder and bowel control.
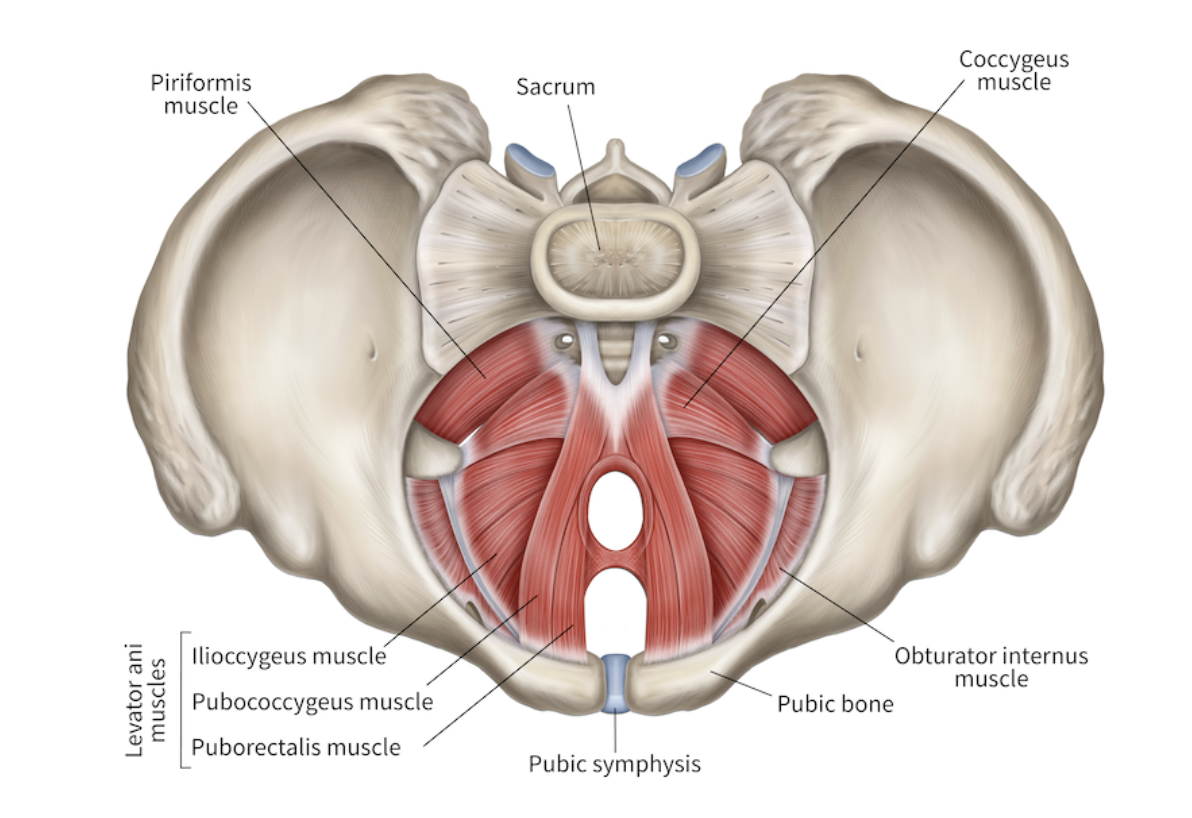
The third layer is the deep layer, also known as the levator ani group. When most people think about their pelvic floor muscles, or hear about them online, these are the ones that are talked about the most. These muscles support the pelvic organs (bladder, rectum, and uterus if you have one). These muscles also play a crucial role in pelvic and spinal stability.
Deep Layer of Pelvic Floor
But wait…there are also accessory muscles!!
There are 2 other important muscles that are not technically pelvic floor muscles, but they are very closely related. These muscles are the piriformis and the obturator internus. These muscles control hip rotation as their main job. However, when they become dysfunctional, they can pull and put tension on the pelvic floor muscles and surrounding structures like the sciatic nerve.
How do these muscles help with bladder and bowel control?
When the pelvic floor muscles contract, pressure is placed around the urethra and rectum to help prevent urine and stool from passing through. Some of these muscles work without you having to think about them (they are under involuntary control). Some of these muscles are also under your control (voluntary control).
So these muscles can help with bladder and bowel control, but what else can they do?
1. Core stabilization and pressure management
These muscles may be small but they play a HUGE role in our stability system. Your core stability system is made up of the pelvic floor muscles at the bottom, the transverse abdominus that wraps around your midsection like a corset, deep stabilizers in between each of the bones in your spine called your multifidus, and your diaphragm.
When you breathe in, your lungs inflate causing the diaphragm to move downward, displacing the abdominal contents in a downward and slightly outward direction. This change in pressure causes the abdominals and low back muscles to stretch and lengthen. The downward pressure also stretches and lengthens the pelvic floor muscles.
When you breathe out, the lungs deflate causing the diaphragm to move upward, the abdominals and spine stabilizers (multifidus) contract, and the pelvic floor muscles contract in an upward direction. This contraction creates a stable pressure within your abdominal cavity and enhances stability so that your body can move from a stable base.
All of these muscles have to be able to relax and contract together to provide maximum stability.
2. Provide support for pelvic organs
The pelvis floor muscles are shaped a little like a bowl to hold the pelvic organs (bladder, rectum, uterus or prostate). Other ligaments and connective tissues provide additional stability to these structures. If dysfunction occurs in the pelvic floor muscles that reduces support, the pelvic organs can start to move in a downward direction. This can lead to something called pelvic organ prolapse.
3. Sexual function
The muscles of the pelvic floor play a crucial role in sexual function. These muscles can help increase sexual sensation, improve ability to achieve orgasm, and reduce discomfort with penetration.
So, do I need to do kegels?
The running joke in my physical therapy program was that professors often answered our many questions the same way: “It depends.” We would all roll our eyes and sigh, but there have never been truer words spoken to me. Whether or not kegels are right for you depends on your unique situation.
Some people have weaker pelvic floor muscles. They have a hard time activating and coordinating these muscles with the other stabilizer muscles. In this case, kegels can be helpful. However, kegels are not the end all be all exercise for the pelvic floor. The pelvic floor muscles also need to coordinate breathing and relaxation with contraction and appropriate timing.
Some people have overactive pelvic floor muscles, which means they are contracted too much. This is also known as a “high tone” or “hypertonic” pelvic floor. Kegels would not be appropriate in this case, and may lead to an increase in symptoms.
How do I know if I should see a pelvic floor therapist?
There are several symptoms or signs that pelvic floor therapy can help with:
Bladder problems:
Weak urine stream
Urinary incontinence with or without exercise
Increased urinary frequency
Difficulty initiating urine stream
Difficulty emptying your bladder
Feeling like you have a UTI, but the urine sample comes back negative for bacteria
Frequent night waking to urinate
Bowel problems:
Straining to have bowel movements
Constipation
Pain during bowel movements
Fecal incontinence
Anal fissures
Hemorrhoids
Sexual dysfunction:
Discomfort during penetrative intercourse
Difficulty achieving orgasm
Pain with tampon insertion
Tailbone pain
Feeling of pelvic pressure of heaviness
Lower back pain
Hip pain
Sacroiliac joint pain
Birth preparation
Postpartum recovery
Diastases recti
What should I expect at my therapy session?
It can be scary or uncomfortable discussing these symptoms with others, let alone a medical provider. Know that a lot of these symptoms are common, and seeing a pelvic floor therapist can help. Feel free to bring someone with you if you feel like it would allow you to be more comfortable.
Step 1: Let’s talk
The first session will consist of a lot of questions about the symptoms you are experiencing, how long they have been going on, and when you notice them the most. The therapist will review your past medical history and gain an understanding of what is most concerning to you and how it is impacting you.
Step 2: Assessment
After talking about the symptoms you find most concerning, your therapist will perform a few different assessments that typically include the following:
External Assessment:
Looking at your overall posture and alignment
Assessing how you breathe
Watch you perform functional movements like bending, squatting, and balancing
Assessing your hip mobility and sacroiliac joint
Assessing any tenderness in your abdomen, diaphragm, back or external hip musculature
Assess for abdominal separation
Assess core stability
Internal Assessment:
This will only be performed with your consent! You also can delay this portion of the exam to a future session if you would like. As you can see from all of the assessments above, your therapist will have a lot of information to work with. Your therapist should continue to assess at your pace and comfort level.
This assessment is different from a gynecological exam. No stirrups or speculum here! The therapist will have you lie on your back and support your hips in a comfortable position with pillows as needed. They will insert a gloved lubricated finger into the vagina and check the pelvic floor muscle for tenderness, strength, and coordination. (An internal rectal assessment is performed for problems with the bowels or tailbone pain, and is also used for those without a vagina or who are unable to do the assessment vaginally.)
This assessment does not take long—just a few minutes and you are all done. The therapist should be talking you through the findings during the examination. If at any time you want to stop or pause the assessment, let your therapist know and they will do so.
Step 4: Developing your personalized treatment plan
After the assessment is complete, the therapist will discuss the information found during the assessment and explain how these findings relate to the symptoms you are experiencing. During this time you may be given exercises to start with at home as well as further discussion about what future treatment sessions will look like to address your concerns.
Summary
The muscles of the pelvic floor play a vital role in stability to allow for more efficient movement patterns throughout your entire body. Pelvic floor therapy can be extremely beneficial for anyone who is experiencing any pelvic pain, low back pain, hip pain, sexual dysfunction, bowel or bladder troubles. The first session may feel a bit overwhelming. However, the therapist’s job is to make you feel heard, comfortable, and respected. They should move at a pace you are comfortable with, educate you on any treatment they think would be beneficial for your symptoms, and always ensure they have your consent.
Written by Kelsey Hight, PT, DPT, COMT